Using Decision Dashboards to guide clinical decisions.
The Busara Clinical Decision Making Framework Intuitive Comparison format
What information visualization is really about is external cognition, that is, how resources outside the mind can be used to boost the cognitive capabilities of the mind. ~ Stuart Card
People can make decisions intuitively, deliberatively, or using a combination of these two methods. Intuitive decisions are made quickly based on habitual and/or emotional responses. They require little cognitive effort but are prone to cognitive biases. Because deliberative decisions involve thought and reflection, they require more time and effort than intuitive decisions. However, they are less susceptible to cognitive biases and other decision traps. [1-3]
Good decision makers, particularly in applied settings, learn how to effectively combine both approaches to take advantage of the strengths and minimize the weaknesses of each. [4] Supporting combined intuitive and deliberative decision making is also an attribute of successfully implemented decision support systems. [5] This is the approach taken in the Busara Clinical Decision Making Framework (BCDMF).
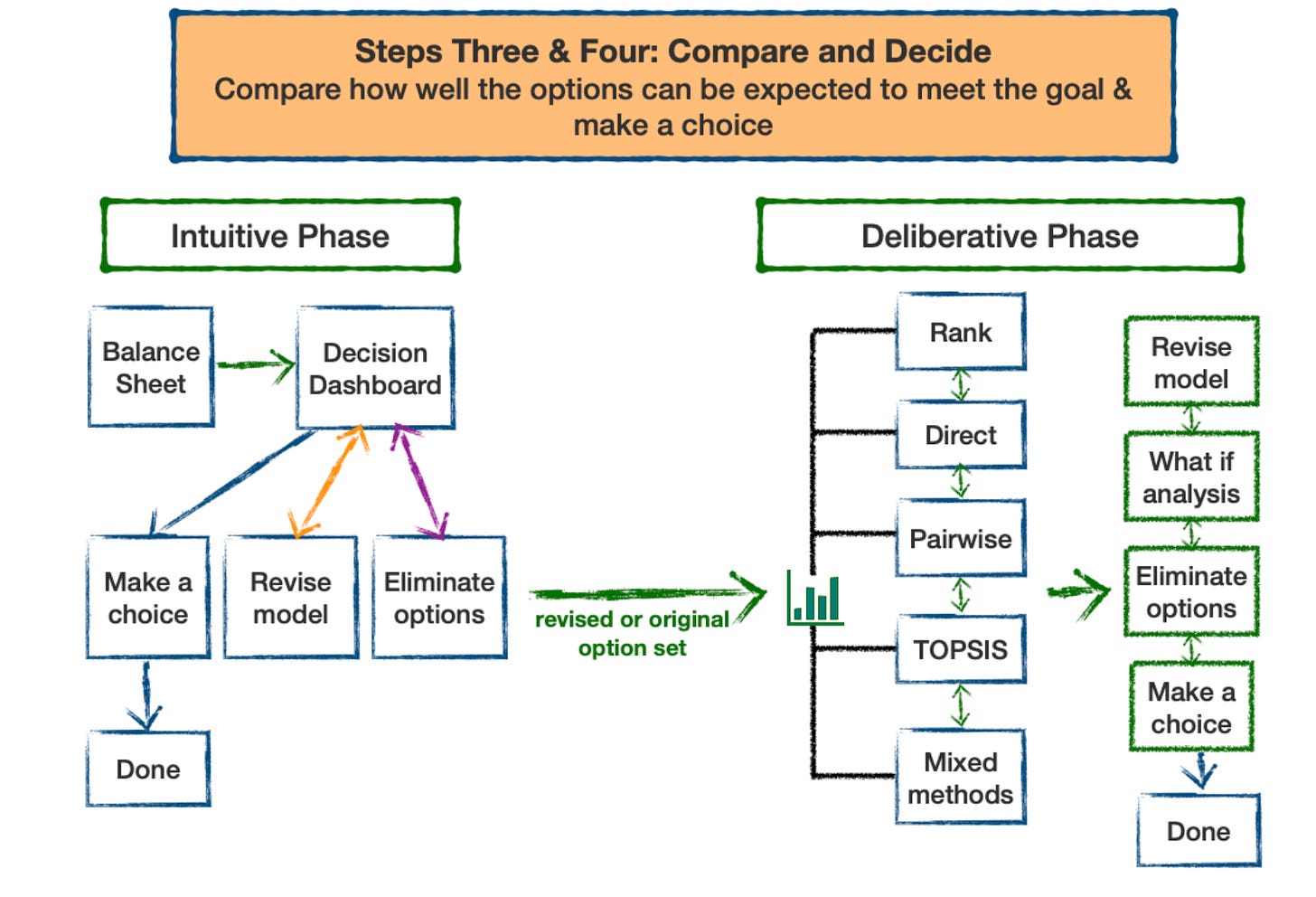
As shown in the figure below, the Comparison and Decide phase of the BCDMF starts with an intuitive phase and then transitions to a deliberative phase if necessary:
I reviewed how to construct and prepare interactive decision dashboards in the March 31, 2023 and April 7, 2023 Musings. Today, I review how they can be used in the BCDMF using a decision dashboard created several years ago comparing options for initial treatment of newly diagnosed, localized prostate cancer. Please note that the data included in the prostate dashboard are old and may not be up to date. Therefore it should be considered an illustration and should not be relied on to make any actual treatment decisions.
Management of newly diagnosed prostate cancer (NDPD)
There are multiple ways to manage NDPD. The four most common are active surveillance (monitoring the course of the disease without intervening), surgery, external beam radiation, and brachytherapy (implanting radioactive pellets in the prostate gland). None of these strategies is clearly better than the others. Therefore the choice of management depends on trade offs between their advantages and disadvantages. At the time the dashboard was created, there was considerable uncertainty about the data regarding the outcomes to be expected with each option. It was therefore important to make clinical decision makers aware of the uncertainties that exist and factor them into their decision making process.
The dashboard developed for men with low risk NDPD is shown below - the link to the interactive version is here.
The dashboard is designed to help people compare the short and longer term benefits and risks of the management options. Benefits are divided into survival rates and the chances that the prostate cancer will not progress. The dashboard also lists information about the three major risks of the management options: sexual, urinary, and gastrointestinal problems. Separate sections of the dashboard are devoted to short term outcomes over the first 5 years and longer term 5 to 15 year outcomes. Users can select which options to display using the menu at the upper right. The menu across the top allows users to select short or long term data and take closer looks at one, two, and four selected outcomes.
One way to use the dashboard is to decrease the number of options by eliminating options that are not desirable based on one or more of their attributes. For example, since the advantages of surgery and external beam radiotherapy are not that different from active surveillance and brachytherapy, one could eliminate them from consideration based on their higher risks of side effects by unchecking them in the options selection panel on the upper right. The resulting dashboard allows one to concentrate on comparing the pros and cons of the two remaining options. See the figure below:
For some, a process like this may be all that is necessary to select a preferred option. Others may want to factor in considerations that were not included in the initial dashboard. In this case, either the initial dashboard would have to be revised to include the new considerations and then reexamined or the decision making process continued without including the new factors in the dashboard display.
Another possibility is that a patient is not yet ready to choose a preferred treatment due to difficulty making one or more of the necessary tradeoffs. In this case, the decision making process would move on to include one or more deliberative decision making methods to help resolve the impasse. I will start to outline how this process could work in the next few Musings.
References
1. Ayal, S., Rusou, Z., Zakay, D., & Hochman, G. (2015). Determinants of judgment and decision making quality: The interplay between information processing style and situational factors. Frontiers in Psychology, 6. https://doi.org/10.3389/fpsyg.2015.01088
2. Kahneman, D. (2003). A perspective on judgment and choice: Mapping bounded rationality. The American Psychologist, 58(9), 697–720. https://doi.org/10.1037/0003-066X.58.9.697
3. Tversky, A., & Kahneman, D. (1974). Judgment under Uncertainty: Heuristics and Biases. Science, 185(4157), 1124–1131. https://doi.org/10.1126/science.185.4157.1124
4. Duke A. Thinking in Bets: Making Smarter Decisions When You Don’t Have All the Facts. New York: Portfolio; 2018.
5. Wu HW, Davis PK, Bell DS. Advancing clinical decision support using lessons from outside of healthcare: an interdisciplinary systematic review. BMC medical informatics and decision making. 2012;12(1):1–10.