Decision quality chain metrics and beyond
Healthcare quality is a function of how well decisions about the care of individual patients are made. The quality of clinical decisions, therefore, is an important, vastly under-appreciated quality metric.
In the December 2, 2022 and January 6, 2023 Musings, I suggested using the decision quality chain, developed by the Strategic Decisions Group (SDG) to help clinical decision makers make good decisions and improve their decision making skills.
The decision quality chain defines a good decision based on six criteria:
A Helpful Frame: A mechanism to clearly define and map the nature and scope of a clinical decision regarding diagnosis or treatment of a patient’s problem.
Clear Values: Inclusion of all important decision-related objectives.
A Comprehensive Set of Alternatives: Identification of a full set of options that could be used to manage the patient’s problem.
Useful information: Ready access to an accurate, trustworthy summary of current evidence in a format designed to support clinical decision making.
Sound reasoning: A process designed to compare alternatives relative to decision objectives, minimize the adverse effects of cognitive biases, cope with decision-related uncertainties, facilitate needed tradeoffs between decision objectives, and allow patients and clinicians (and other appropriate parties) to discuss each other’s decision-related preferences and priorities.
Commitment to follow through: Willingness of both patient and provider to implement the chosen alternative.
Additional information about the Decision Quality Chain is available on the SDG website and in the book Decision Quality. [1,2]
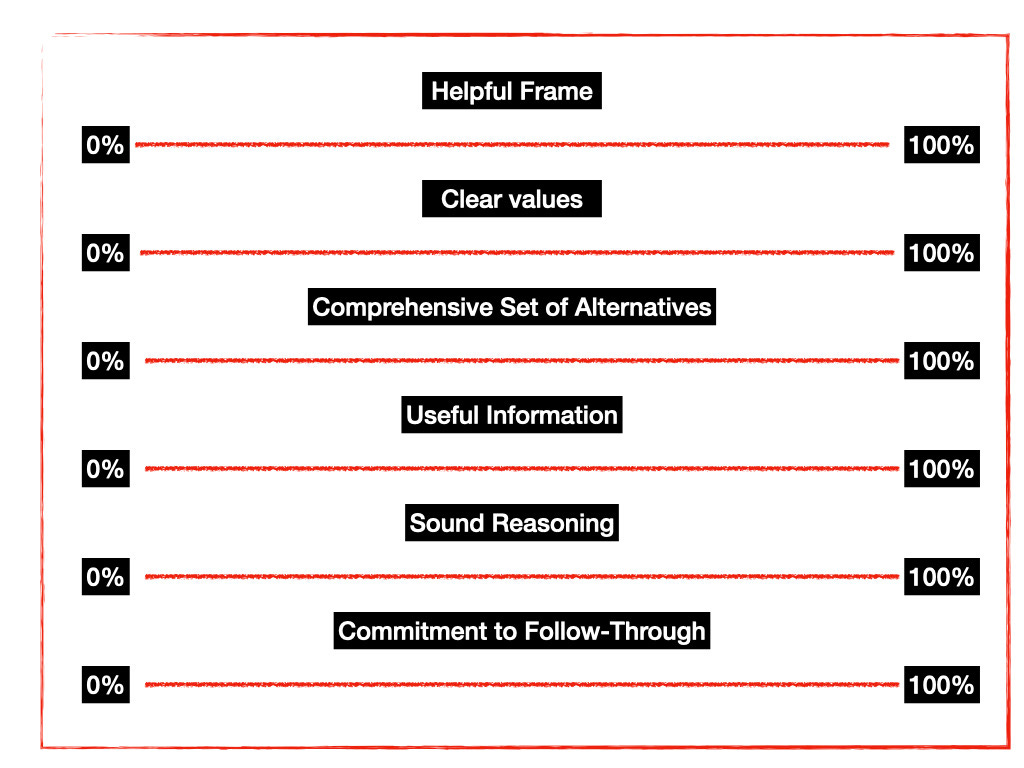
Using this framework, SDG created a simple evaluative tool to help decision makers measure the quality of their decision making processes. The tool consists of rating how well each component of the decision quality chain has been satisfied on a scale from 0 to 100%. A sample tool, adapted from the free version available for download on the SDG website, is shown below.
This tool is best used by decision makers to guide an ongoing decision making process. Collection and analysis of the final decision quality evaluations made by providers and patients would be an especially meaningful quality metric by creating a learning feedback loop to identify which of the six quality criteria they have the least confidence in and, therefore, are the most problematic. These areas could then be targeted for quality improvement efforts.
In addition to using the decision quality chain to guide and evaluate the quality of decisions, SDG and the Society of Decision Professionals have used it to develop a set of “Decision-Maker’s Rights” stating that every decision maker deserves the opportunity to make a quality decision. A copy of these rights can be downloaded from the SDG website.
This statement does an excellent job of defining what patient-centered, shared decision making means. I’d love to see if it proves to be more effective than the current descriptions of shared decision making that, according to current research, clinicians have found confusing or redundant. (See, for example, Elwyn 2017 [5] and Melzer 2020 [6]).
Here is an initial attempt to modify these rights to make them a list of what patients faced with an important health-related decision should expect to receive from their provider:
A decision frame that structures the decision in terms of individual patient values, preferences, social situation, and health status.
A set of alternatives that include the full range of options available.
Ready access to relevant, reliable, and understandable information that incorporates the uncertainties that exist.
Help in understanding the potential outcomes of each alternative described in terms of their individual values and preferences.
Help in making a choice based on sound reasoning and analysis.
Interaction with a clinician who is able to ensure that these expectations are met and who will support and enable commitment to the preferred course of action.
Musings
I have seen several recently published articles highlighting the need to develop a workable metric to measure the quality of clinical decision making. [3,4] Rather than re-inventing the wheel, I see no reason why the decision quality chain metric could not be used for this purpose. Doing so would focus attention on the importance of measuring and improving the clinical decision process in real time. It would also serve to improve the decision making skills of providers and patients. I think it is time to stop treating the issue of decision quality as solely an item of pure academic research and start using the excellent tools already available to improve the ongoing process of health care.
It is worth noting that the decision quality chain metric can also be used to guide the deliberations of clinical guideline creators and others involved in the design and provision of health care. Good health care depends on good decisions at all levels of the health care system.
References
1. Decision Quality Book Resources | Strategic Decisions Group [Internet]. SDG. Available from: https://sdg.com/decision-quality-book-resources/
2. Spetzler, Carl, Winter, Hannah, Meyer, Jennifer. Decision Quality: Value Creation from Better Business Decisions [Internet]. New York: Wiley; 2016
3. Hamilton JG, Lillie SE, Alden DL, Scherer L, Oser M, Rini C, et al. What is a good medical decision? A research agenda guided by perspectives from multiple stakeholders. J Behav Med. 2017 Feb 1;40(1):52–68.
4. Lu Y, Elwyn G, Moulton BW, Volk RJ, Frosch DL, Spatz ES. Shared Decision Making in the U.S.: Evidence exists, but implementation science must now inform policy for real chang to occur. Zeitschrift für Evidenz, Fortbildung und Qualität im Gesundheitswesen. 2022 May;S1865921722000824.
5. Elwyn G, Durand MA, Song J, Aarts J, Barr PJ, Berger Z, et al. A three-talk model for shared decision making: multistage consultation process. BMJ. 2017;359:j4891.
6. Melzer AC, Golden SE, Ono SS, Datta S, Crothers K, Slatore CG. What Exactly Is Shared Decision-Making? A Qualitative Study of Shared Decision-Making in Lung Cancer Screening. J Gen Intern Med. 2020;35(2):546-553.